Understanding Syphilis
Introduction
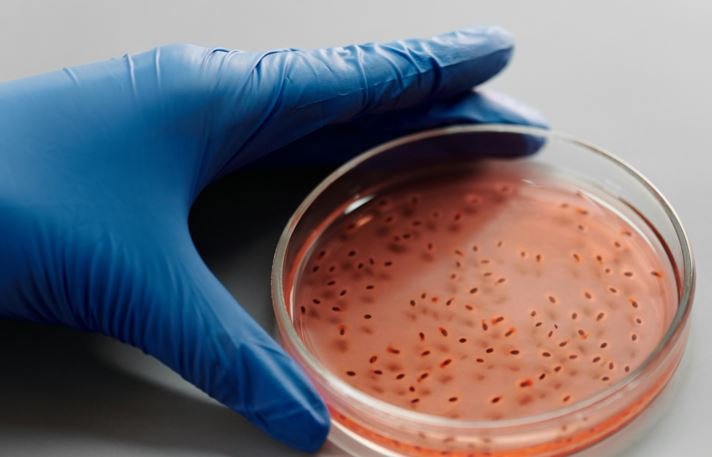
Syphilis, a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, has been a persistent public health challenge for centuries. Known for its diverse clinical manifestations and serious long-term consequences if left untreated, syphilis remains a topic of significant medical and social importance. This blog aims to provide a thorough understanding of syphilis, including its history, stages, diagnosis, treatment, and prevention.
A Brief History of Syphilis
Syphilis has a long and storied history, with its first major outbreak recorded in Europe in the late 15th century. Known as the “great pox” to differentiate it from smallpox, it caused widespread fear and suffering. The disease was often associated with moral judgment and stigma, which complicated efforts to address it publicly and scientifically. The discovery of Treponema pallidum by Fritz Schaudinn and Erich Hoffmann in 1905 was a pivotal moment in understanding the disease, leading to the development of effective treatments and preventive measures.
The Stages of Syphilis
Syphilis progresses through distinct stages, each with characteristic signs and symptoms:
- Primary Syphilis:
- Symptoms: The primary stage is marked by the appearance of a chancre, a painless ulcer that typically develops at the site of infection (genitalia, rectum, or mouth) about three weeks after exposure.
- Diagnosis: During this stage, Treponema pallidum can be detected directly from the chancre using dark-field microscopy or PCR.
- Secondary Syphilis:
- Symptoms: This stage, occurring weeks to months after the initial infection, is characterized by skin rashes (often on the palms and soles), mucous membrane lesions, fever, swollen lymph nodes, and other systemic symptoms.
- Diagnosis: Blood tests for antibodies against Treponema pallidum are typically positive at this stage.
- Latent Syphilis:
- Symptoms: Latent syphilis has no symptoms and is divided into early latent (within the first year) and late latent (after the first year) stages. The bacterium remains in the body, and the infection can be detected only through blood tests.
- Diagnosis: Latent syphilis is diagnosed based on a history of positive syphilis tests without symptoms.
- Tertiary Syphilis:
- Symptoms: If untreated, syphilis can progress to the tertiary stage years after the initial infection. This stage can cause severe complications, including gummas (soft tissue swellings), cardiovascular syphilis, and neurosyphilis (affecting the brain and spinal cord).
- Diagnosis: Diagnosis of tertiary syphilis may involve serological tests, imaging studies, and examination of cerebrospinal fluid.
Diagnosis
The diagnosis of syphilis involves a combination of clinical evaluation and laboratory testing:
- Serological Tests: These include non-treponemal tests (such as the Rapid Plasma Reagin (RPR) and Venereal Disease Research Laboratory (VDRL) tests) and treponemal tests (such as the fluorescent treponemal antibody absorption (FTA-ABS) and Treponema pallidum particle agglutination (TP-PA) tests).
- Direct Detection: In primary syphilis, direct detection of Treponema pallidum from lesions can confirm the diagnosis.
- Neurological Examination: For suspected neurosyphilis, cerebrospinal fluid analysis is essential.
Treatment
Penicillin remains the cornerstone of syphilis treatment:
- Primary, Secondary, and Early Latent Syphilis: A single intramuscular injection of benzathine penicillin G is usually sufficient.
- Late Latent and Tertiary Syphilis: Requires multiple doses of benzathine penicillin G over several weeks.
- Neurosyphilis: Treated with intravenous penicillin G for 10-14 days.
For those allergic to penicillin, alternative antibiotics such as doxycycline or tetracycline may be used, although desensitization to penicillin is often preferred for neurosyphilis.
Prevention
Preventing syphilis involves a combination of strategies:
- Safe Sexual Practices: Using condoms and having mutually monogamous relationships with uninfected partners.
- Regular Screening: Routine testing for high-risk populations, including sexually active individuals, pregnant women, and those with multiple partners.
- Education: Public health campaigns to raise awareness about syphilis transmission and prevention.
Conclusion
Syphilis, though an ancient disease, continues to pose significant health challenges. Early diagnosis and effective treatment are crucial in preventing the severe complications associated with advanced stages. Through public awareness, safe sexual practices, and regular screening, the burden of syphilis can be significantly reduced, ensuring better health outcomes for affected individuals.
By understanding the history, stages, diagnosis, treatment, and prevention of syphilis, we can better combat this enduring public health issue.
Supported by factual information, sound reasoning, and You included specific examples and you organized should be impacted positively.
Information you shared is authentic I checked it online.I am big fan of your writing skills.
impressive